Abstract
Background: Collectively, non-Hodgkin lymphomas (NHL) are expected to account for >95,000 new cancer diagnoses and >24,000 cancer deaths in the United States in 2018. Few NHL risk factors are known other than severe immune compromise, family history of lymphoid malignancies, and some pathogens. Evidence for modifiable risk factors that could inform prevention strategies is limited, especially from prospective studies. An association of anthropometric traits with NHL risk is biologically plausible given the emerging knowledge that obese individuals have heightened inflammation and deregulation of endogenous hormonal pathways that can influence cell cycle control and lymphocyte activation. We undertook the present prospective study to elucidate the associations of young (aged 18-21 years) and usual adult body mass index (BMI), height, weight, and waist circumference with risk of NHL and major histologic subtypes of NHL. The completed analysis will leverage the resources of several large population samples across the United States with prospectively assessed repeated measures of anthropometric traits and high rates of follow-up for disease ascertainment.
Methods: We pooled data from large prospective cohort studies with repeated measures of anthropometric traits and follow-up over 23 - 38 years for cancer endpoints, including the Cancer Prevention Study-II (CPS-II) Nutrition Cohort, Health Professionals Follow-up Study (HPFS), Nurses' Health Study (NHS), and NHS II. Incident NHL diagnoses were confirmed by review of medical records or cancer registries, and classified for histologic subtype according to the WHO classification scheme and corresponding InterLymph-recommended analytic groups: chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL), and T-cell NHL (T-NHL). Weight was ascertained approximately every two years throughout follow-up, all other anthropometric measures were ascertained on a single survey, usually at baseline. We considered cumulative average of BMI (hereafter "usual adult BMI") by averaging across all completed cohort-specific questionnaires. Current weight was analyzed as time-varying. In cohort- and sex-specific analyses, there was no evidence of statistically significant heterogeneity; thus we pooled directly across cohorts to maximize our sample size for statistical modeling. Cox proportional hazard regression models adjusted for age, cohort, and sex were used to estimate hazard ratios (HR) and 95% confidence intervals (CIs) for each trait's association with NHL or NHL subtype risk.
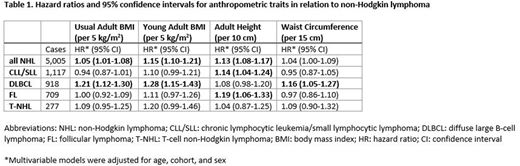
Results: The pooled sample comprised 5,005 confirmed incident cases of NHL, including 1117 CLL/SLL, 918 DLBCL, 709 FL and 277 T-NHLs ascertained over 9.4 million person-years of follow-up. There was a significant, positive association of usual adult BMI with NHL overall (HR: 1.05, 95% CI: 1.01-1.08 per 5 kg/m2; Table 1), which was driven by DLBCL (HR: 1.21, 95% CI: 1.12-1.30 per 5 kg/m2). No association was apparent for FL, CLL/SLL or T-NHL. Similarly, waist circumference was associated with NHL risk overall (HR: 1.04, 95% CI: 1.00-1.09 per 15cm), but driven by the association for DLBCL (HR: 1.16, 95% CI: 1.05-1.27 per 15cm). In contrast, a statistically significant or suggestive association for BMI in young adulthood was observed for all NHL endpoints, but again, most strongly with DLBCL (HR: 1.28, 95% CI: 1.15-1.43 per 5 kg/m2). Height was positively associated with all NHL endpoints except T-NHL. Associations for current and young adult weight were similar to those for the corresponding BMI variables.
Conclusions: Preliminary results from this prospective analysis suggest that, unlike BMI later in life, young adult BMI is consistently associated with all major subtypes of NHL. In contrast, usual adult BMI and waist circumference are uniquely associated with DLBCL. In general, the strongest associations with anthropometric factors were observed for DLBCL. Further analyses of these data are ongoing, including efforts to incorporate data from two additional large cohorts. These findings further demonstrate the etiologic heterogeneity of NHL subtypes and underscore the importance of maintaining a healthy body weight throughout life, including at younger ages.
Chao:Seattle Genetics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal